Summary (TL;DR):
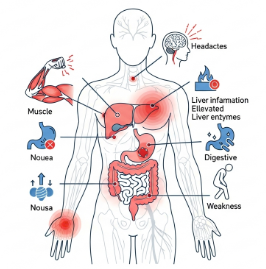
Statins are highly effective for reducing cardiovascular events, but like all medications they have adverse effects. The most commonly discussed are muscle symptoms (SAMS), mild liver enzyme elevations, a small increase in diabetes risk, and rare serious events (rhabdomyolysis, clinically significant liver injury). Recent large analyses show that true statin-caused muscle pain is less common than perceived, but patient-reported intolerance remains a major adherence barrier. Management relies on careful assessment, dose/formulation adjustment, rule-out of other causes, and evidence-based rechallenge strategies. Some supplements (CoQ10) have been tested but meta-analyses show inconsistent benefit. Panax ginseng may offer general antioxidant and metabolic support, but evidence for preventing or treating statin side effects is limited and there are rare case reports of interactions — discuss with your clinician before combining. Wiley Online Library+4The Lancet+4Taylor & Francis Online+4
1) How common are statin side effects? (what the data show)
- Adverse-event reporting vs trial data: Randomized controlled trials (RCTs) generally report relatively low excess risk of serious adverse events from statins; observational and post-marketing surveillance report more events because of larger, more diverse populations. A recent pooled analysis of many trials reported that, while muscle symptoms occur, the absolute excess risk attributable to statins is small for most people — many reported muscle aches are comparable to placebo rates once blinded trial data are pooled. Large-scale trial analyses have emphasized that statins’ cardiovascular benefits greatly outweigh these risks. The Guardian+1
- Muscle symptoms (SAMS): Prevalence estimates vary widely. Clinical series and meta-analyses report prevalence from a few percent to ~10% depending on definitions and patient selection; true statin-caused myopathy (CK elevation >10× ULN, rhabdomyolysis) is rare (<0.1%). Recent focused reviews estimate SAMS as the leading cause of discontinuation and intolerance, but causality assessment is critical because many non-statin causes of myalgia exist. Taylor & Francis Online+1
- New-onset diabetes: Large meta-analyses and trial data show a modest increase in the risk of new-onset diabetes (relative risk increase roughly 9–13% in some meta-analyses), concentrated in people with preexisting metabolic risk; yet statins’ cardiovascular risk reduction remains strongly favorable even accounting for this diabetes signal. A recent Lancet analysis reaffirmed the diabetes risk but emphasized net cardiovascular benefit. PubMed+1
- Liver enzyme elevations / hepatotoxicity: Mild transaminase elevations are relatively uncommon and usually transient. Clinically significant statin-induced liver injury (DILI) is rare — population studies report rates on the order of tens of cases per 100,000 person-years; severe cases are very uncommon but have been documented. Routine frequent liver enzyme monitoring is not indicated for most patients; baseline testing and targeted follow-up if symptoms or risk factors are present is recommended. PMC+1
- Cognitive effects: Reports of memory problems and confusion exist and were acknowledged by regulatory agencies (FDA labeling changes). Large observational and trial-based reviews find no consistent long-term cognitive harm, though rare reversible cognitive complaints have been reported and typically resolve after stopping the drug. Current guidance is cautious but not prohibitive. U.S. Food and Drug Administration+1
2) Biological mechanisms behind common statin side effects
Muscle-related (SAMS) mechanisms:
- Statins inhibit the mevalonate pathway, reducing not only cholesterol but intermediates required to synthesize coenzyme Q10 (CoQ10) — a mitochondrial electron carrier — potentially impairing mitochondrial function in muscle.
- Statins may alter muscle cell membrane composition, calcium handling, or induce low-grade inflammation in susceptible individuals.
- Genetic variants (e.g., SLCO1B1 polymorphisms) and drug interactions (CYP3A4 inhibitors) raise statin muscle toxicity risk by increasing statin plasma levels. Wiley Online Library+1
Glucose metabolism (diabetes risk):
- Statins may slightly impair insulin sensitivity or secretion via effects on beta-cell function and peripheral glucose uptake; the absolute increase in diabetes risk is small but notable in high-risk individuals. Mechanistic work continues. PubMed
Liver effects:
- Statin metabolism in the liver can elevate transaminases in some patients; idiosyncratic DILI is rare and likely immune-mediated in susceptible people. Distinguish this from benign, transient enzyme rises. PMC
Cognitive reports:
- Mechanistic explanations are uncertain; proposed hypotheses include altered cholesterol metabolism in the CNS or off-target effects. Evidence remains inconclusive and cognitive complaints are typically reversible. PMC
3) Clinical definitions and diagnostic approach to adverse effects (practical research-based framework)
Statin-Associated Muscle Symptoms (SAMS) — spectrum:
- Myalgia: muscle ache/weakness without CK elevation.
- Myopathy: muscle symptoms with CK elevation (typically >4× ULN used clinically; >10× ULN is more serious).
- Rhabdomyolysis: severe muscle breakdown with very high CK, myoglobinuria, risk of renal failure (very rare). Taylor & Francis Online+1
Evaluation checklist (evidence-informed):
- Symptom characterization (onset relative to statin start/dose change, symmetry, exercise relation).
- Check CK, renal function, and TSH (hypothyroidism mimics myopathy).
- Review concomitant medications that raise statin levels (CYP3A4 inhibitors, fibrates) and substance use (alcohol, grapefruit).
- Consider alternative causes (vitamin D deficiency, polymyalgia rheumatica, musculoskeletal disease).
- If CK normal and symptoms mild, consider temporary cessation or lower dose and rechallenge; many patients tolerate alternative statins or dosing schedules. Detailed management algorithms are available in clinical guidance. AHA Journals+1
4) Evidence for prevention or treatment of statin side effects
Coenzyme Q10 (CoQ10):
- Multiple randomized trials and meta-analyses have tested CoQ10 for statin myalgia; pooled results are inconsistent and most meta-analyses have not shown robust, reproducible benefit. Guidelines do not universally endorse its routine use for SAMS, though some clinicians try it empirically given low risk. PubMed+1
Statin switching / dose adjustment / intermittent dosing:
- Switching to a different statin (e.g., pravastatin or rosuvastatin) or lowering dose can reduce muscle complaints. For patients intolerant to daily dosing, alternate-day or twice-weekly high-intensity statin regimens have been trialed with partial success under close supervision. AHA Journals
Non-statin lipid-lowering therapies:
- Ezetimibe, PCSK9 inhibitors, bempedoic acid, and other agents can be used when statins are not tolerated; combinations may achieve LDL targets while minimizing statin exposure. Choice depends on risk, cost, and availability. AHA Journals
5) Drug interactions and special cautions
CYP3A4 substrates and inhibitors: many statins (simvastatin, lovastatin, atorvastatin) are metabolized by CYP3A4. Concomitant use of strong CYP3A4 inhibitors (certain azole antifungals, macrolide antibiotics, protease inhibitors, grapefruit juice) can raise statin levels and toxicity risk. Guidelines list clinically significant interactions and dose limits. AHA Journals+1
Fibrates (gemfibrozil): increase risk of myopathy when combined with statins — avoid gemfibrozil with statins; fenofibrate is often preferred if combination is needed but monitor closely. PMC
Anticoagulants and antiplatelets: some statin interactions can affect bleeding risk indirectly; careful monitoring advised when combined with warfarin or antiplatelet therapy. AHA Journals
6) Statins & diabetes: what clinicians should know
- The absolute increase in diabetes risk is modest; risk is concentrated in people with pre-existing risk factors (prediabetes, obesity, metabolic syndrome). In most high-risk cardiovascular patients, statins’ benefits (reduced heart attacks/strokes) outweigh the diabetes risk. Monitor fasting glucose or HbA1c periodically, especially in high-risk patients. PubMed+1
7) Liver safety: recommended monitoring based on evidence
- Baseline liver function tests (ALT/AST) are recommended before starting statin therapy. Routine periodic testing in asymptomatic patients is not universally required; repeat testing is indicated if symptoms suggest hepatic injury (fatigue, abdominal pain, jaundice) or if transaminases become markedly elevated. Clinically significant statin-induced liver injury is rare. PMC
8) Cognitive effects: current evidence and guidance
- The FDA acknowledged rare reversible cognitive effects and updated labeling. However, systematic reviews and large RCT follow-ups show no consistent, long-term cognitive harm attributable to statins; reported cognitive complaints are typically reversible on discontinuation. Clinicians should evaluate cognitive symptoms for other causes and consider statin trial discontinuation with clinician guidance if symptoms are bothersome. U.S. Food and Drug Administration+1
9) Role of genetics and precision prescribing
- Genetic variants (most notably SLCO1B1 *c.*521T>C) are associated with higher statin exposure (especially simvastatin) and increased myopathy risk. Genetic testing can inform personalized statin selection/dosing in patients with prior intolerance or family history. Precision approaches are increasingly integrated into practice for high-risk or intolerant patients. Wiley Online Library
10) Panax (Korean) Ginseng — supportive role and interaction cautions
What the research says (supportive, not curative):
- Panax ginseng contains antioxidant and anti-inflammatory ginsenosides and has been shown in some clinical and preclinical studies to improve markers of endothelial function, support glucose metabolism, and reduce oxidative stress — mechanisms that could theoretically mitigate some contributors to statin side effects (oxidative muscle damage, metabolic stress). However, no high-quality RCT demonstrates that ginseng prevents or treats statin myopathy or other statin adverse effects directly. Use ginseng only as a supportive supplement, after discussing with your healthcare provider. PMC+1
Interaction risk:
- Though uncommon, case reports exist of adverse interactions between ginseng and statins (e.g., a reported possible liver injury when ginseng was combined with atorvastatin). Herbal-drug interactions can be unpredictable due to variability in herbal preparations and potential effects on drug-metabolizing enzymes or transporters. For example, some herbs alter CYP enzymes or transporter proteins impacting statin pharmacokinetics. Always use standardized products and tell your clinician about any supplements. Wiley Online Library+1
Practical points if considering ginseng while on statins:
- Use high-quality, third-party tested products.
- Start with a low dose and report any new symptoms (muscle pain, dark urine, jaundice) immediately.
- Avoid combining with other substances known to raise statin levels (grapefruit).
- Monitor LFTs and CK if indicated by symptoms or clinician judgment. Wiley Online Library+1
11) Best-practice management algorithm (evidence-based summary)
- Baseline: document indication for statin, baseline lipids, fasting glucose/HbA1c, LFTs, CK if prior muscle disease.
- Onset of symptoms: assess temporality, check CK/renal function, evaluate other causes (thyroid, vitamin D, exercise), review drug interactions. Wiley Online Library
- Mild symptoms + normal CK: consider temporary discontinuation to see if symptoms resolve, then rechallenge with same or different statin, or reduce dose / use alternate-day dosing.
- Moderate/severe symptoms or CK >4× ULN: stop statin, monitor CK and renal function, investigate rhabdomyolysis if clinically suspected.
- Persistent intolerance: consider non-statin lipid lowering (ezetimibe, PCSK9 inhibitors, bempedoic acid) and discuss cardiovascular risk trade-offs. AHA Journals
12) Research gaps and future directions
- Better-designed RCTs focusing on patient-reported muscle outcomes with standardized definitions and objective measures (CK, mitochondrial markers) are needed.
- High-quality studies of CoQ10, exercise interventions, and herbal adjuvants (including standardized Panax ginseng preparations) for SAMS are required — current evidence is inconsistent. PubMed+1
13) Practical takeaways for patients & clinicians
- Do not stop statins abruptly without consulting your clinician; untreated high LDL poses real cardiovascular risk.
- Report any new muscle, cognitive, or hepatic symptoms promptly.
- Most statin adverse effects are manageable through dose/formulation changes, switching agents, or using alternative lipid-lowering therapies if needed.
- Be transparent about supplement use (including ginseng); herb-drug interactions are possible and product quality varies.
- Share family history, other medications, and lifestyle factors so your clinician can personalize therapy safely. AHA Journals+1
14) Key references & further reading (selected)
- FDA safety communication on statins (labeling; cognition, LFTs). U.S. Food and Drug Administration
- Recent Lancet and large-scale analyses of statin benefits and diabetes signal. The Lancet
- Comprehensive reviews on SAMS, pathophysiology, and management. Taylor & Francis Online+1
- Statin-induced liver injury clinical review. PMC
- Meta-analyses on CoQ10 and statin myopathy (no conclusive benefit). PubMed+1
- Guidance on drug–drug interactions and management. AHA Journals+1
- Case report noting possible atorvastatin–ginseng hepatic interaction; review of herb–drug interactions. Wiley Online Library+1